Ontario hospital's proposed plan to treat patients in critical care misses the mark, union argues
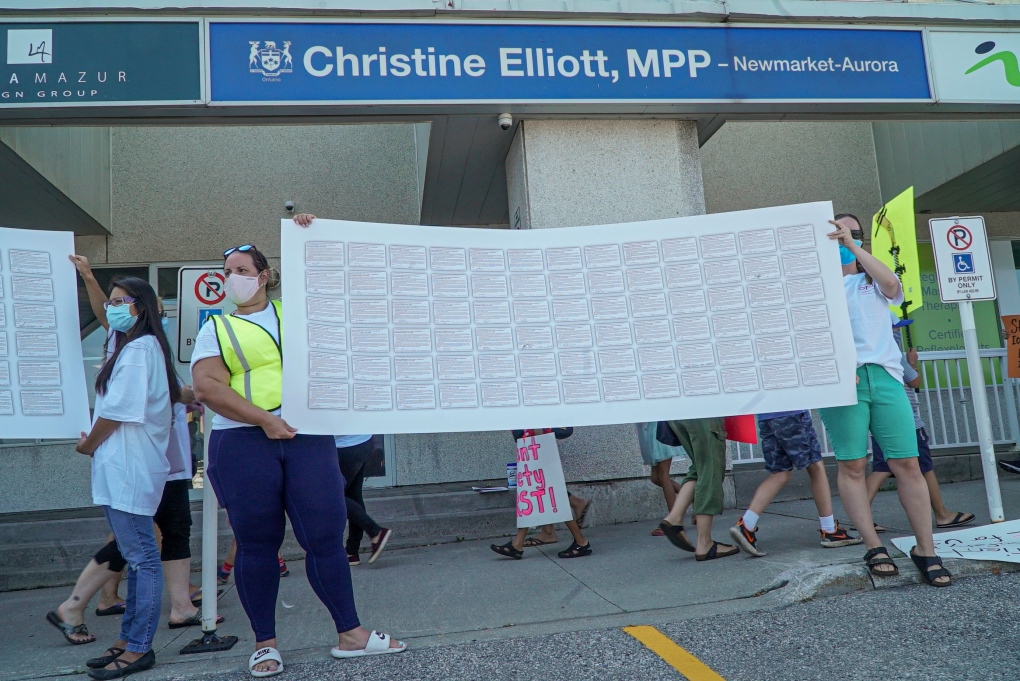
 A protest is seen outside Health Minister Christine Elliott's constituency office in Newmarket on August 31, 2021. (Gregory Bennett/Ontario Nurses’ Association)
A protest is seen outside Health Minister Christine Elliott's constituency office in Newmarket on August 31, 2021. (Gregory Bennett/Ontario Nurses’ Association)
A Newmarket hospital’s plan to implement a team-based approach to critical care will put patients at risk, according to Ontario’s largest nursing union.
The Ontario Nurses Association (ONA), which represents 68,000 nurses and health-care professionals across the province, argues that Southlake Regional Health Centre’s proposed “team-based nursing” model -- which would see a RN [registered nurse] working with a team of other health-care practitioners to deliver care to multiple patients as opposed to the current one-to-one nurse-to-patient ratio -- will lead to the “erosion of quality critical care” at the facility.
“Team-based nursing is something that came up in the 80s, and maybe very early 90s, but was done away with in so many different scenarios because it does have a number problems,” DJ Sanderson, a registered emergency room nurse employed by Southlake with experience in its ICU, told CTV News Toronto over the phone last week. Sanderson is currently on leave from those duties as he serves on the ONA’s board of directors.
“In an ICU scenario, I’m not sure how Southlake envisions that happening. You need this one-to-one dedicated care with a qualified, registered nurse to be able to assess, reassess, and initiate any sort of rapid intervention that’s required for these sorts of patients.”
Moreover, the ONA said that Southlake’s response to what it calls a “RN staffing crisis in its intensive care unit” is to hire RNs without providing full education and training in critical care prior to these nurses working in the ICU.
Back in July, the ONA said that Southlake’s board of directors had denied its request from RNs and registered respiratory therapists (RRTs) to address the risks the staffing model would pose to patient care.
A month later, ICU nurses and RTTs at Southlake delivered hundreds of postcards to Health Minister Christine Elliott, who represents the riding of Newmarket–Aurora where the hospital is located, to demand intervention on the issue.
Since then, some 4,300 people have signed a petition by the ONA to axe the program and the topic has made its way into the provincial legislature a handful of times over the last two weeks alone.
Most recently, Nickel Belt MPP and NDP Health-Care Critic France Gelinas pushed Elliott during question period last Monday to “listen to the concern of her constituents” and act to ensure that every patient admitted to the ICU gets “nothing less” than the standard one-to-one nurse-to-patient ratio.
“Southlake, like all hospitals in Ontario, has seen eight years of budget freeze or below inflation increase,” Gelinas said at the time. “They have adopted a team-based nursing model in their ICU, that means that now, the one, fully-trained ICU RN monitors her patients, but she must also monitor RNs who are not trained in critical care nursing. That is not one-on-one, Speaker. That is not best practice.”
In response, Elliott said that there are “always” qualified intensive nurses in Southlake’s ICU and that they will always provide supervision of anyone who has “not achieved that status.”
“There are qualified professionals in every aspect of our health-care system, including intensive care with the appropriately trained nurses, and that will always continue,” Elliott said.
For Sanderson, he argues that Elliott “completely side-stepped the question.”
“As the Minister of Health, am I expecting her to have in-depth knowledge of what’s happening exactly on the ground in the ICU at Southlake? No. But whoever has been giving her her information about the state of nursing at Southlake, and the state of nursing in Ontario, I’m really concerned with her broad statement that we’ll always have critical care nurses there when you need it. That’s just not the reality,” Sanderson said.
In an email to CTV News Toronto, the Ministry of Health said that health-care organizations are responsible for making their own decisions when it comes to the clinical needs of their patients.
“In the case of hospitals, the board is ultimately responsible for the management of their operations, including issues associated with patient care,” a spokesperson for the ministry said.
According to a report released last month by Ontario’s Science Advisory Table, which has been guiding the provincial government throughout the COVID-19 pandemic, 9,096 Ontarians have been admitted to an ICU with COVID-19-related critical illness since March 20, 2020.
“The COVID-19 pandemic has strained Ontario’s critical care system. At the peak of wave 3, the number of patients on ventilators was over 180 per cent of pre-pandemic historical averages,” the report read.
The table added that the only reason Ontario’s critical care system was able to accommodate the influx was by deferring surgeries and procedures, funding new ICU beds and “identifying temporary surge space, team-based care models utilizing redeployed staff.”
“The critical care system does not currently have capacity to accommodate a surge as it did during waves 2 and 3 due to worsening staffing shortages, healthcare worker burnout, and health system recovery efforts.”
On Dec. 7, the table released new modelling data which showed that Ontario will see a rise in COVID-19 cases as well as hospitalizations even without the Omicron variant.
“We can’t predict Omicron precisely, but it will almost certainly hit us hard and fast,” the scientists said in a series of messages on Twitter. “Cases are rising, even without much Omicron yet. Our hospitals and ICUs are feeling pressure again. We need to increase vaccination and we can’t let up on public health measures.”
That prediction is especially worrying for Sanderson, who said that nurses are exhausted and may not be fully prepared for yet another wave of COVID-19 infection in Ontario’s hospitals.
“They need a break and to move right into another wave so quickly, without any opportunity to rest and recharge, I really worry,” Sanderson said.
“Of course, as nurses, we’re going to do absolutely everything we can to be there for the patients of Ontario. But, it’s really concerning about what the next wave could bring, if the numbers they project do come to light.”
In an email to CTV News Toronto, Southlake spokesperson Kathryn Perrier said that to date, the hospital has not implemented a new team-based nursing model in its ICU and no nurses have worked in the ICU to care for a patient independently prior to having received the proper training.
Perrier added that, despite the provincial nursing shortage that is impacting hospitals across the province, the hospital confirmed it would not move forward with accepting any new entrants into its pre-sponsorship program, which sees newly hired RNs provide extra support to existing ICU nurses in advance of completing the critical care training program, a move which Sanderson applauded.
“In order to continue to provide the quality of care our community expects and deserves, we have developed a comprehensive plan to recruit and retain staff. As a result of the province-wide nursing shortage and after 21 months of the pandemic, hospitals are working to rebuild their workforces and expanding the pipeline for new nurses is the responsible thing to do. Closing beds in our ICU is not a viable option, given the needs of the rapidly growing and aging communities we serve,” Perrier said.

CTVNews.ca Top Stories

Stamp prices rise for the third time in five years amid financial woes for Canada Post
Canada Post is increasing stamp prices for the third time since 2019, a move the Crown corporation says is a "reality" of its sales-based revenue structure.
BREAKING Winnipeg man admits to killing four women, claims he's not criminally responsible
Defence lawyers of Jeremy Skibicki have admitted in court the accused killed four Indigenous women in Winnipeg, but argues he is not criminally responsible for the deaths by way of mental disorder – this latest development has triggered a judge-alone trial rather than a jury trial.
Trudeau Liberals to unveil new bill Monday aimed at countering foreign interference
Democratic Institutions Minister Dominic LeBlanc will be tabling legislation on Monday aimed at countering foreign interference in Canada. Federal officials have scheduled a technical briefing on the incoming bill for Monday afternoon.
WATCH Avian flu: Risk to humans grows as outbreaks spread, warns expert
H5N1 or avian flu is decimating wildlife around the world and is now spreading among cattle in the United States, sparking concerns about 'pandemic potential' for humans. Now a health expert is urging Canada to scale up surveillance north of the border.
Human remains were found at a former Hitler base, but decay prevents determining the cause of death
Polish prosecutors have discontinued an investigation into human skeletons found at a site where German dictator Adolf Hitler and other Nazi leaders spent time during the Second World War because the advanced state of decay made it impossible to determine the cause of death, a spokesman said Monday.
Italy's white-collar mafia is making a business killing
Italy's mafia rarely dirties its hands with blood these days. Extortion rackets have gone out of fashion and murders are largely frowned upon by the godfathers.
Ontario MPP asked again to leave Ontario legislature over keffiyeh, Speaker loosens ban
An Ontario MPP was asked again to leave the Ontario legislature on Monday for wearing a keffiyeh, a garment that was banned by the Speaker last month due to its political symbolism.
The story of how a B.C. man found his birth mother
After his adopted parents died, Dave Rogers set out to learn more about his birth mother. DNA results and a little help from friendly strangers would put him on a path to a small town in England.
Trump fined US$1,000 for gag order violation in hush money case as judge warns of possible jail time
The judge presiding over Donald Trump's hush money trial fined him US$1,000 on Monday for violating his gag order once again and sternly warned the former president that additional violations could result in jail time.






























