'This is about racism:' 72-year-old Black woman says she was 'humiliated' at Ontario hospital
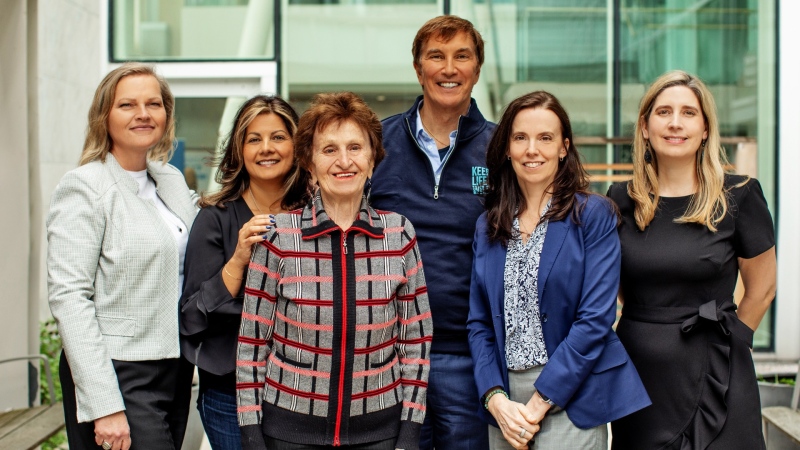
 Shirley Archibald is photographed with her family (Supplied).
Shirley Archibald is photographed with her family (Supplied).
A 72-year-old Black woman said she felt “humiliated” and “intimidated” while trying to seek treatment for her heart condition at an Ontario hospital last week.
“I started feeling like my heart was going to stop,” Shirley Archibald told CTV News Toronto.
On Feb. 8, she headed to the emergency department at Windsor Regional Hospital.
In the past, she had suffered from atrial fibrillation, which causes the heart to quiver and escalates the risk of a stroke or heart failure. Last Tuesday, she started to experience familiar symptoms.
“Everything would go black,” Archibald said. For support, she called her daughter, Amie Archibald-Varley, a registered nurse in the Hamilton-Niagara region.
At the hospital, her pain deepened. Archibald-Varley told her mother over the phone to walk up to the registration window and inform a health-care professional. “The girl literally yelled at me and said, ‘Go sit down,’” Archibald said.
About 15 minutes later, the registration clerk notified Shirley that a triage nurse was available to speak with her. But when she explained that her daughter was on the phone for support, Archibald said the nurse screamed, “If you don’t turn off your phone, I’m going to call security.”
“I started crying,” Archibald said. “She’s yelling at me in this vulnerable place where I have no one with me and I’m really scared.”
Meanwhile, she looked around and noticed other patients sitting in the waiting room talking on their cell phones. “Why was it that my mom specifically was being targeted in the way she was being treated?” Archibald-Varley said.
At this point in time, she told her mother to place her phone in her purse, but advised her not to hang up. From there, Archibald-Varley said, “I could hear this nurse and the security guard yelling at my mom.”
“The intimidation, the threatening, the bringing security into it. The mistreatment was more than enough to force my mom out of the hospital,” Archibald-Varley said.
On the curb outside, Archibald said she cried like a baby.
Eventually, she received the treatment she needed, which she said was due in large part to her daughter’s outspoken advocacy. “If Amie was not there for me, would I have been left on the curb to die?”
In response, Windsor Regional Hospital (WRH) and the Ontario Nurses Association (ONA) said in a joint statement, “WRH and ONA take any allegation of discrimination very seriously. This particular situation continues to be reviewed carefully with the benefit of all the facts including the input of nursing staff and other information.”
“We will advocate to safeguard the reputation of our nursing staff who have worked diligently and with integrity throughout this pandemic to care for Ontarians in their time of need.”
“This is about racism,” Archibald-Varley said. “This is about the discriminatory treatment of racialized people. There is so much evidence that supports that racialized people tend to have poorer health-care outcomes than the general population.”
Longstanding research – paired with the mistreatment of Joyce Echaquan, John River and Dominic Hookimaw – has served as ample evidence of the inequities that push Black and Indigenous people to fall through the cracks of the Canadian health-care system.
In all three cases, each Black or Indigenous patient said they were insulted, overlooked or a victim of violence, resulting in a poor health outcome. In Echaquan’s case, the tragic result was fatal for the Indigenous woman.
An Ontario Ministry of Health spokesperson said the province is committed to “ensuring equality” within the health-care system “so that no one is treated with bias based on their gender or race.”
“We have to remember that our health system does not treat everyone equally,” said Dr. Naheed Dosani, health equity lead at Kensington Health in Toronto. “The poor experiences of racialized people in Canadian healthcare has been going on for a very long time.”
Echoing that sentiment, Dr. Andrew Baback Boozary, executive director of social medicine at Toronto's University Health Network, said, “The reality is that the system has shut out so many. There has been a history of marginalization and mistrust with active systemic racism taking place within the health-care system.”
“Unfortunately, we have seen so many tragic instances take place over the last few years pre-pandemic and concurrently,” Boozary said.
Archibald-Varley worries about the patients who don’t have sufficient support and who walk away from the hospital without returning.
“How many other people might have had very poor healthcare outcomes because they didn't have someone to advocate for them? How many people might have died under the system because they didn't have the support?” Archibald-Varley said.
“I think those are some of the other questions we really need to start asking ourselves as a collective society in terms of how we address these issues.”
CTVNews.ca Top Stories

Doctors concerned about potential spread of bird flu in Canada
H5N1 or avian flu has been detected at dozens of US dairy farms and Canadian experts are urging surveillance on our side of the border too.
There's a limit to how much interest rates in Canada and U.S. can diverge: Macklem
Bank of Canada governor Tiff Macklem says Canadian interest rates don't have to match U.S. or global rates, but there is a limit to how much they can diverge.
Prince William and Kate release photo of daughter Charlotte to mark ninth birthday
Prince William and his wife Kate released a picture of their daughter Charlotte to mark the princess's ninth birthday on Thursday.
This Canadian restaurant just lowered its prices. Here's how it did it
A Canadian restaurant lowered its prices this week, and though news of price tags dropping rather than climbing sounds unusual, the business strategy in this case is not, according to experts in the field.
Should I invest with a human or a robot? Traditional firms vs. robo-advisors
Investors considering where to park their money have a choice: go with a traditional financial adviser or trust in an algorithm. Here are the pros and cons of both.
Five human skeletons, missing hands and feet, found outside house of Nazi leader Hermann Goring
Archeologists have unearthed the skeletons of five people, missing their hands and feet, at a former Nazi military base in Poland.
As Hamas considers ceasefire, question hangs: Will Israel end war without the group's destruction?
Hamas on Thursday was considering the latest proposal for a ceasefire with Israel that the United States and other mediators hope will avert an Israeli attack on the Gaza town of Rafah.
Imagine living in a 4-foot body that doesn't develop chronic diseases
Nathaly Paola Castro Torres has a rare disorder called Laron syndrome that is caused by a genetic mutation. It stunts her growth but also provides a hidden silver lining: Her body is protected from chronic diseases such as cancer that often take life away long before old age.
Concerns about Plexiglas prompt inspections at some Loblaws locations in Ottawa
Inspections are underway at more than one Loblaws location in Ottawa after complaints were filed about tall Plexiglas barriers.