TORONTO -- Patients with the greatest chance of survival beyond 12 months should be prioritized for critical care in the event that overwhelmed Ontario hospitals need to begin rationing life-saving treatments, the provincial government said in a document sent to hospitals earlier this month.
The province’s triage protocol guidance states that patients should be assessed and placed in a colour-coded framework based on their risk of short-term mortality, which is defined as survival beyond 12 months after the onset of critical illness.
“In the context of a major surge in demand for critical care resources, where the demand actually exceeds the number who can be safely managed with available resources (including ventilators, supplies and trained staff), it is inevitable that some who may have otherwise benefited from critical care will not receive it, and as a result, some will die who would otherwise have lived,” reads the province’s triage protocol document, dated Jan. 13, 2021.
“In such a context, an emergency standard of care is appropriate in order to mitigate the worst effects of this surge. This document represents an emergency standard of care that aims to reduce preventable deaths to the degree possible.”
According to the document, patients with a short-term mortality risk of 80 to 99 per cent should be labelled “red,” those with a 50 to 79 per cent risk should be labelled “purple.” Those with a short-term mortality risk of 30 to 49 should be categorized as “yellow” and patients with a risk of 1 to 29 should be labelled “green.”
The province states that in a “level 1 triage scenario,” patients who have a greater than 20 per cent chance of surviving twelve months should be prioritized and in a “level 2 scenario,” those with a greater than 50 per cent chance should be prioritized for care.
“Under a Level 2 triage, the hospital and regional authorities should continue to coordinate transportation of patients and resources to optimize the utilization of all critical care resources before initiating a level 3 triage,” the document reads.
In a “level 3 triage scenario,” those with a greater than 70 per cent chance of surviving 12 months should be prioritized for critical care.
“At level 3 triage patients who have suffered a cardiac arrest will be deprioritized for critical care, as their predicted mortality is greater than 30 (per cent). Thus, Code Blue may no longer be called for cardiac arrest, and out-of-hospital cardiac arrests may not be transferred to hospitals in Level 3 triage,” the document states.
All patients being considered for critical care treatment must be assessed by two physicians and if a consensus about the patient’s mortality risk is not reached, the more optimistic prognosis will be selected.
“If demand for critical care continues to exceed available resources at Level 3, there may be little clinical evidence to guide triage decisions on the basis of predicted short term mortality. As a result, triage decisions must appeal to procedural fairness,” the document concludes.
“If triage decisions must be made between multiple patients who cannot be distinguished on the basis of predicted short term mortality, a system of random selection among eligible and not-yet-admitted patients should be implemented by an administrator on call.”
Patients should be assessed “on an ongoing basis,” according to the document.
“ICU physicians should also reassess patients admitted to ICU at regular intervals, and consider withdrawal of life support through a shared decision-making process with SDMs (substitute decision-makers) if a patient does not appear to be improving despite receiving critical care,” the document continues.
The province has not said at what point hospitals will have to implement the triage protocol but speaking to CP24 last week, Dr. Michael Warner, the medical director of critical care at Michael Garron Hospital, said with around 400 COVID-19 patients in intensive care units around the province, that day could soon be coming.
"Once we get to the 550 number, which we will exceed for sure, that is where a potential triage protocol could be implemented whereby patients who are more likely to survive their COVID-19 or other illness will be given life support preferentially over others if those resources are not available for everybody," he said.
The chair of the province’s science table said last week that about 25 per cent of all Ontario hospitals have no available ICU beds while another 25 per cent only have one or two remaining.
The province’s latest modelling released last Tuesday indicated that with three per cent case growth, Ontario hospitals could see 1,000 COVID-19 patients in intensive care by early February.
It should be noted that over the past week, COVID-19 case growth in Ontario has significantly slowed.
“We are at a dangerous point,” epidemiologist Dr. Adalsteinn Brown, co-chair of the province’s COVID-19 science table, said while releasing the modelling last week.
"As we climb closer to 1,000 intensive care beds, about half of our capacity filled with COVID-19 patients in February, we will have to confront choices that no doctor ever wants to make and no family ever wants to hear.”
Ontario NDP Leader Andrea Horwath accused the Ford government of keeping the triage protocol document “secret.”
“This document shows us all that we are on the path to heart-wrenching choices and devastating loss if we don’t make this lockdown count with stronger measures — paid sick days, more help in long-term care, and in-workplace and in-school testing,” Horwath said in a written statement released Monday.
“People that are loved dearly — people that need medical help the most — could be left to die if we do not make the choice to throw everything we’ve got at this virus.”
The Accessibility for Ontarians with Disabilities Act Alliance (AODA Alliance) also released a statement on Monday, outlining “dire concerns” they have about the protocol’s impact on those living with disabilities.
The group said setting a patient’s 12-month likely survival as the benchmark risks further discrimination against those living with disabilities.
“People with disabilities have been disproportionately exposed to the risk of getting COVID-19, and of suffering its most serious impacts,” David Lepofsky, chair of the AODA Alliance, said in a written statement.
“Compounding this cruel reality, this secret document shows that some patients with disabilities now risk being de-prioritized in access to life-saving critical care that they will disproportionately need if Ontario hospitals, now near the breaking point, cannot provide life-saving critical medical care to all patients needing it.”
The document sent to hospitals stresses the need to consider Ontario’s Human Rights Code when considering decisions on prioritizing care.
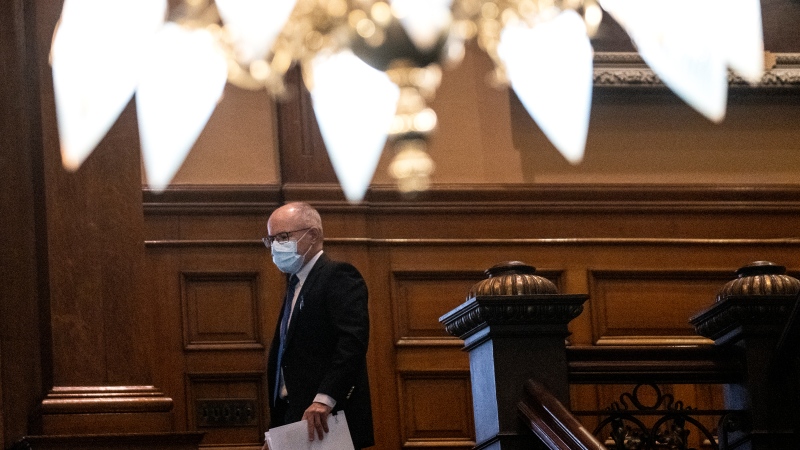
Speaking about the triage guidance at a news conference on Monday, Dr. David Williams, the province’s chief medical officer of health, said provincial officials hope that the protocol never has to be implemented.
“You don’t want to think of it in the heat of it, you want to lay these things out ahead of time. So I think they’ve done that with the hope of saying, we hope to never have to use this,” Williams said.
“I think that they are moving it around to look at because you want to have all of the different ones weigh in with their commentary... It’s hard to get a group of doctors in a room together to agree on everything and it is better if you socialize that and get the input and the collective knowledge and wisdom in a worse-case scenario hoping that it’s not something you are going to pull off the shelf.”
He said the province remains in a “precarious” position when it comes to ICU capacity.
“That is just one of the many things that is being done throughout the whole sector to prepare for... different scenarios that we are going to have to face as now our ICU beds are over that 400,” he said.
He noted that the province hopes to eventually bring the number of COVID-19 patients in ICU down below 150.
“That’s where the modellers said we could get back to doing all of the other procedures at the same time. That is a target to head for. I think we can get there,” he said.
“But it’s uncertain... we are plateauing but that doesn’t mean we can’t jump up again because places like the UK, and others, plateaued and then went up very rapidly when the UK variant took off.”