COVID-19 in Ontario: What you need to know as we head into fall and winter
Following a summer with relatively little worry over COVID-19, infection numbers are once again starting to trend upward ahead of the official start of fall this weekend.
While Ontario is better positioned to deal with the virus now, officials are saying that the public still has a role to play in stopping the spread of COVID-19 and other respiratory illnesses, which can have serious consequences for some people as well as the health-care system.
Here’s what you need to know about where we are with COVID-19 in Ontario now and the outlook for the months to come.
WHERE WE ARE NOW WITH COVID-19?
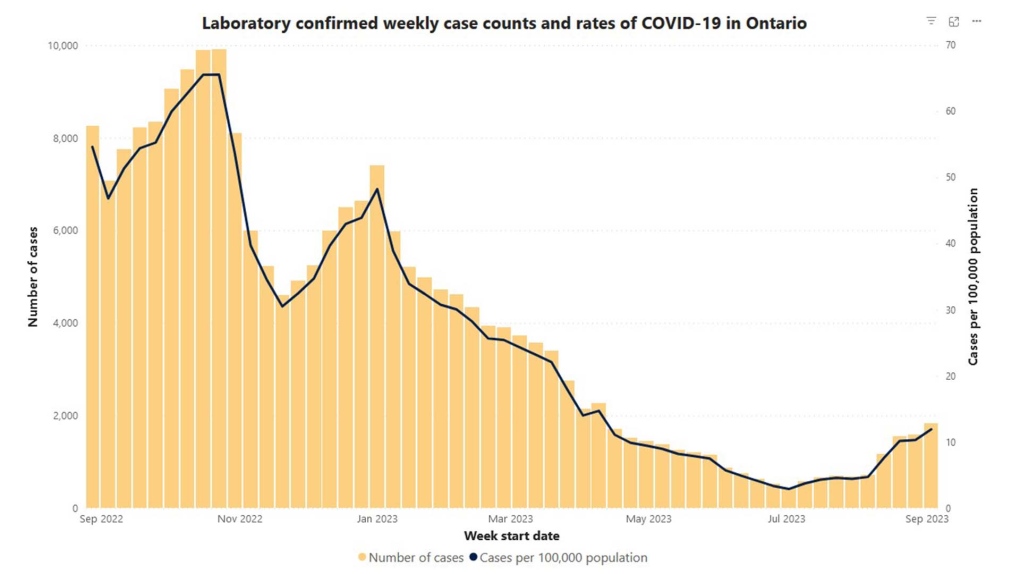
According to data from Public Health Ontario, case numbers have been climbing since hitting a low point in early July. For the first full week of September, Ontario saw roughly 12 cases per 100,000 people. That's up from the roughly three cases per 100,000 people at the low point in July, but still a far cry from the roughly 47 cases per 100,000 people the province saw at the same time last year. These numbers, however, significantly underestimate the true number of infections as they are based on the results of PCR or rapid molecular testing, which only a portion of the public qualifies for.
Positivity has also been trending upward recently, sitting at around 14.1 per cent the first week of September, up sharply from the 4.8 per cent low near the end of June, according to data from the Provincial COVID-19 Diagnostic Network. Wastewater data, which monitors virus levels found in sewage and is in some ways a more accurate depiction of COVID-19 activity, show the virus is on the rise within the general population.
- Download our app to get local alerts on your device
- Get the latest local updates right to your inbox
Outbreaks are also increasing at long-term care homes, hospitals, and retirement homes.
“It (COVID-19) is clearly spreading quite rapidly right now,” Dr. Fahad Razak told CP24.com in an interview, noting that in addition to the data indicating a rise, many people are anecdotally reporting outbreaks tied to gatherings and testing positive for the first time ever.
But Razak, an internist at St. Michael’s Hospital and the former scientific director of the Ontario COVID-19 Science Table, says there's an important distinction to make between the rising COVID-19 cases that we are seeing now compared to the past few years.
Importantly, the number of COVID-19 patients in the ICU has remained fairly stable, sitting at around 22 in Ontario for the last week of August. So while cases are on the rise, fewer people are becoming seriously ill.
“So notably, there's really been no meaningful rise in the number of people in ICU or on ventilators,” Razak said. “So remember, going back to 2020, 2021, the really severe COVID infections we saw were that classic COVID pneumonia presentation where people would come in, oxygen levels were low, rapidly deteriorating, and they'd go into the intensive care unit.
“And so while this rise is happening, this time we're not seeing that and I can say clinically, we're not seeing that as well. And that reflects the fact that the population — Canadians, people in Ontario — there's a lot of immune protection already in place.”
Widespread vaccinations coupled with previous rounds of infection mean that fewer people are getting seriously ill when they get infected, he noted.
“What we call hybrid immunity is doing its job. So it's protecting the majority of people who are getting infected from having severe outcomes,” Razak said. “Now, that's something to be celebrated. So I think along with this rise of infections, you have to acknowledge the significant, the better position we are in now versus where we were a couple of years ago.”
However there’s a caveat.
SO WHAT’S THE OUTLOOK FOR THIS SEASON?
While there is more immunity in the community now, some of that immunity is waning, given how long it's been since many people had their last vaccine dose or infection. Just 4.1 per cent of those five and older who completed their primary COVID-19 vaccine series have had a booster shot within the last six months, according to government figures.
And while most people aren't getting as sick from COVID-19, the illness still poses a threat to those who are older, or who have weakened immune systems.
As well, a rise in COVID-19 case numbers could compound with rising influenza and RSV cases to pose a threat to the health-care system, as was the case last year when Ontario experienced a "triple whammy" of the three diseases, which overwhelmed hospitals.
“I think we'd have to anticipate that the probability is we will experience that once again,” Razak said. “So knowing that, the protective strategies become especially important. So whatever can be done to reduce the burden of infections so that we can reduce that strain on the health-care system, I think that becomes really, really important.”
That’s where vaccines come in.
 A staff member at a vaccine clinic looks outside the clinic for people waiting to get their COVID-19 vaccine or flu shot during the COVID-19 pandemic, in Mississauga, Ont., on Wednesday, April 13, 2022. THE CANADIAN PRESS/Nathan Denette
A staff member at a vaccine clinic looks outside the clinic for people waiting to get their COVID-19 vaccine or flu shot during the COVID-19 pandemic, in Mississauga, Ont., on Wednesday, April 13, 2022. THE CANADIAN PRESS/Nathan Denette
WHO SHOULD GET A VACCINE AND WHEN?
Ontario is expected to start receiving the most up-to-date COVID-19 vaccines targeting the latest variants in September. Public health officials have said that the vaccine will be made available first to those in the highest risk groups, including those who are older, or who have underlying health conditions.
While there is not currently a strong recommendation for people who are younger and relatively healthy to get the latest vaccine, it will eventually become available to everyone six months and up and the more people who get it, the stronger the protection for the overall community.
Ontario’s influenza shot will become available in September to those at highest risk, including hospitalized individuals, hospital staff and residents and staff in long-term care homes, followed by those in retirement homes and other congregate settings. Starting Oct. 30, the shot will become available to the entire population six months and older.
Ontario is also rolling out its first RSV vaccination campaign, making the RSV vaccine Arexvy available to those 60 years and older living in long-term care homes, Elder Care Lodges, and for some retirement home residents.
Razak notes that getting a vaccine, even if you are not in a high-risk group, helps reduce the overall spread, which in turns helps protect the strained health-care system.
“It's not like we've had a significant influx of doctors or nurses. We don't have dramatically new hospital capacity this year than we did last year. And last year was a period of very significant strain,” he said.
He recalled that 2022 saw records across the country in terms of wait times in emergency rooms, shutdowns of the emergency rooms and deferral and delays of other critical procedures, surgeries, and imaging tasks.
“All of these were delayed as we had these waves of disease come in. So I think it's on all of us, on all Canadians to try and reduce the strain on the health-care system as much as possible because if the health-care system is overwhelmed, it's not just COVID, it's cancer surgeries or treatments. It's a knee replacements. It's a severe car accident where there's an emergency room that doesn't have the capacity to manage people as quickly as it needs to.
“So protecting the health-care system means protecting it for all of us. And so avoiding COVID infections but also getting your flu vaccine on RSV vaccine for people who are high risk. These are part of the preventative strategies that I think are going to be key to keeping our system working well over the following winter.”
WILL WE NEED TO WEAR MASKS THIS FALL AND WINTER?
There are few settings left in Ontario where masking is a requirement. While masking was mandated as a way to prevent infection during the initial waves of the pandemic, public guidance has shifted to masking as a personal choice.
That said, there are still a number of places where it is recommended, such as on public transit. And there are many places and circumstances, Razak said, where it just makes sense.
“Think of it as an adaptive strategy,” he said. “This is part of reducing risk during periods of high spread. It's not forever, it's only for the few weeks to maybe a couple of months where those waves are occurring. We're clearly in a wave right now.”
He said masking during periods of high transmission is considered common courtesy in many Asian countries and he said similar behaviour here could help stop the spread of respiratory illness.
“I don't think we are in a policy environment where a mask mandate is possible, nor should it be required unless we're at a critical, critical state,” Razak said. “But behavioral change, people doing things to protect themselves and those around them, I think that's something that many of us do.”
He likened a change in thinking around masking to cultural shifts around drinking and driving and seatbelt use over the past few decades.
“Really, the reason people wear seatbelts most of the time now is not because they think that they're going to get ticketed, it's because it's just this thing that you do to reduce risk,” he said. “So masking is a good comparison to that.”
He added that masking in hospitals and other health-care settings, especially given staffing shortages, could be a significant early strategy to reduce spread and protect the system.
While there might not necessarily be mandates, Razak said government and organizations should encourage people to do things that help reduce spread, such as having plentiful supplies of masks and hand sanitizer available for people who wish to use them around subways, hospitals, schools and other settings.
WHAT IF YOU DO GET COVID?
Those who do get a COVID infection this season should stay home until they are feeling better and wear a tight-fitting mask in public settings for 10 days from the onset of symptoms. Those at high risk of severe outcomes from COVID-19 are able to access free PCR testing at pharmacies.
Anyone with severe symptoms, such as shortness of breath or chest pain, should seek medical treatment, informing your provider ahead of time that you have COVID-19.
According to Toronto Public Health, people can return to work, school, and everyday activities when you have no fever and your symptoms have been improving for at least 24 hours.
“If you're infected and you’re in a high risk group, remember to get tested and that there are medications like Paxlovid which have an important role in reducing the risk of severe disease and long COVID,” Razak said. “And so that should be something that people seek out as much as possible.”
CTVNews.ca Top Stories

Most Canadians have heard about Freeland's resignation from Trudeau cabinet, new poll finds
The majority of Canadians heard about Chrystia Freeland's surprise resignation from Prime Minister Justin Trudeau's cabinet, according to a new poll from Abacus Data released Tuesday.
BREAKING 2 B.C. police officers charged with sexual assault
Two officers with a Vancouver Island police department have been charged with sexual assault, authorities announced Tuesday.
Canadian government announces new border security plan amid Donald Trump tariff threats
The federal government has laid out a five-pillared approach to boosting border security, though it doesn't include specifics about where and how the $1.3-billion funding package earmarked in the fall economic statement will be allocated.
Police chief says motive for Wisconsin school shooting was a 'combination of factors'
Investigators on Tuesday are focused on trying to determine a motive in a Wisconsin school shooting that left a teacher and a student dead and two other children in critical condition.
B.C. teacher disciplined for refusing to let student use bathroom
A teacher who refused to let a student use the bathroom in a B.C. school has been disciplined by the province's professional regulator.
Fall sitting bookended by Liberal byelection losses ends with Trudeau government in tumult
The House of Commons adjourned on Tuesday, bringing an end to an unstable fall sitting that has been bookended by Liberal byelection losses. The conclusion of the fall sitting comes as Prime Minister Justin Trudeau's minority government is in turmoil.
After investigating Jan. 6, House GOP sides with Trump and goes after Liz Cheney
Wrapping up their own investigation on the Jan. 6 2021 Capitol attack, House Republicans have concluded it's former GOP Rep. Liz Cheney who should be prosecuted for probing what happened when then-President Donald Trump sent his mob of supporters as Congress was certifying the 2020 election.
The world's busiest flight routes for 2024 revealed
If you think planes have got fuller and the skies busier over the past year, you’d be right — especially if you live in either Hong Kong or Taipei.
Prosecutors charge suspect with killing UnitedHealthcare CEO as an act of terrorism
The man accused of killing UnitedHealthcare's CEO has been charged with murder as an act of terrorism, prosecutors said Tuesday as they worked to bring him to a New York court from from a Pennsylvania jail.