TORONTO -- An online calculator that would help Ontario doctors decide which patients should be treated and which should be turned away COVID-19 cases overwhelm hospitals is meant to be used as a last resort, says an ethics consultant involved in its design.
The “Short-term mortality risk calculation tool” takes in age and medical conditions, and outputs scores that can help a doctor determine the likelihood that a patient will survive for a year if treated.
If that threshold is low — the bed that could have gone to that patient can be given to someone more likely to survive.
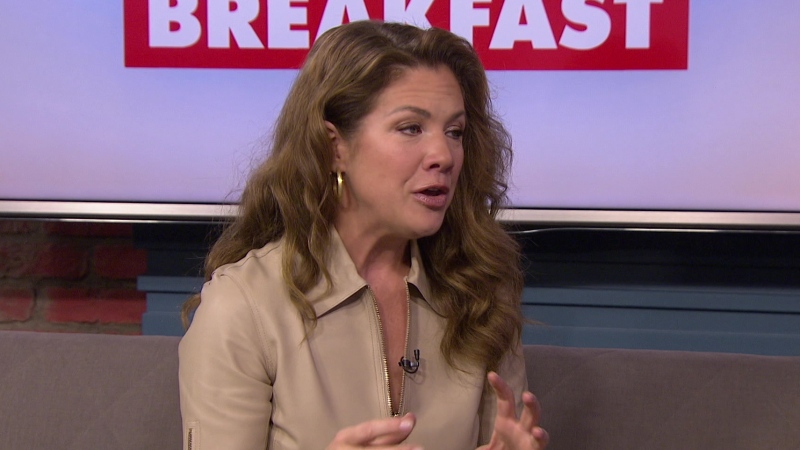
“The calculator, to be very clear, is not driving the clinical decision. The calculator simply helps the physician at the bedside to check the accuracy of the clinical judgment,” said Dr. Andrea Frolic of Hamilton Health Sciences.
But that hasn’t quelled worries of advocates for people with disabilities, who say that ingrained in the assessment tools it digitizes are biases against people in wheelchairs or people whose life span may not be clear.
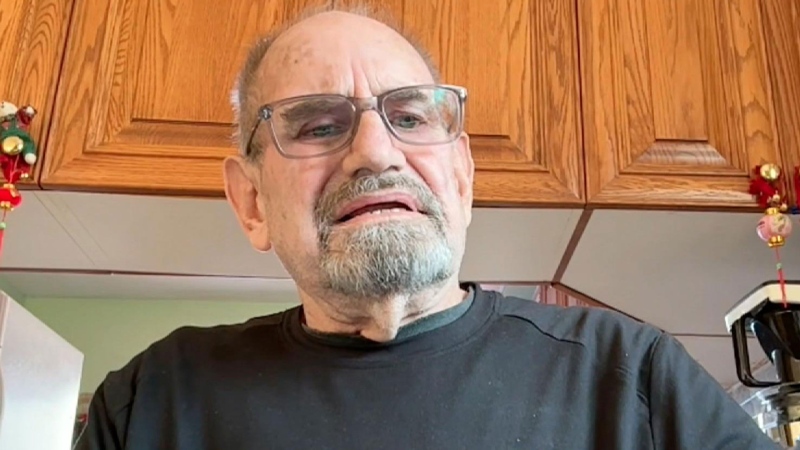
“The calculator dehumanizes it and makes it falsely seem like it’s a mathematical calculation. It is not,” said David Lepofsky of the AODA Alliance, an Ontario disability advocacy group.
He pointed to elements of the “ECOG Grade” that included a score for “Completely disabled; cannot carry on any self-care; totally confined to bed or chair.”
“People with disabilities are disproportionately exposed to getting COVID, and dying of COVID. It would be a cruel irony if they then faced the risk of being deprioritized in getting access to critical care,” Lepofsky said.
The STMR Calculation Tool is a digital expression of the “Short Term Mortality Risk Assessment for Critical Illness” form that doctors may have to fill out if they are overwhelmed. That form was obtained by CTV News Toronto.
In a “Level 1 Triage Scenario,” patients with a greater than 80 per cent chance of dying in the next year are turned away. In Level 2, that drops to 50 per cent. In Level 3, patients with just a 30 per cent chance of dying could be turned away.
Among the list of conditions that could meet that criteria are severe trauma, burns, cardiac arrests, metastatic cancers, strokes, and liver failure.
The form includes a line of age greater than 65, and “Clinical Frailty Score” of greater than seven on a nine-point scale. It cautions doctors that this frailty must be part of a progressive illness, and not an ongoing condition.
All of those criteria were pulled from global medical literature designed to determine the chance that someone would survive a year, Dr. Frolic said.
“Great pains have been taken to ensure that equality, that any patient with any diagnosis gets the same assessment applied, to mitigate any potential bias,” she said.
It’s not immediately clear who is behind the online calculator. There’s no logo on the website, and a check of its domain registration shows “redacted for privacy” on many identifying details.
However in the site’s end user license agreement, the site mentions the “Hamilton Health Sciences Corporation” — an agency of Hamilton Health Sciences. That was where the programming was done for the tool, which was commissioned as part of Ontario’s COVID-19 response, said Dr. Frolic.
Ottawa Centre MPP Joel Harden, who is the NDP Critic for accessibility and persons with disabilities, said there had been little public discussion of what end of care life should be.
“We have a government operating in secrecy on critical life or death decisions. If the hospitals get overwhelmed the government will not debate out in the open what the criteria should be in rationing lifesaving care,” Harden said.
The Ontario Ministry of Health did not return messages left by CTV News Toronto.