TORONTO -- It was in 2014 that Toronto resident Mark Farrant was called to serve as a juror for a very graphic murder trial. But in carrying out his civic duty, he paid a terrible price. He developed Post Traumatic Stress Disorder.
“You saw autopsy photos, detailed photos of the victim, of the crime scene. Very detailed photos of the wounds and this was a very violent homicide,” says Farrant.
He thought his mental distress would decline after the trial but it only accelerated. And he found himself becoming suicidal, believing the world would be better off without him.
The problem was that jurors are sworn to secrecy. And that included talking to medical professionals about what they experienced in a trial.
“I started to reach out, even to my own family physician,” he recalls. “Door after door after door kept closing.”
In 2014, jurors could only get mental health treatment if it was authorized by the trial judge themselves.
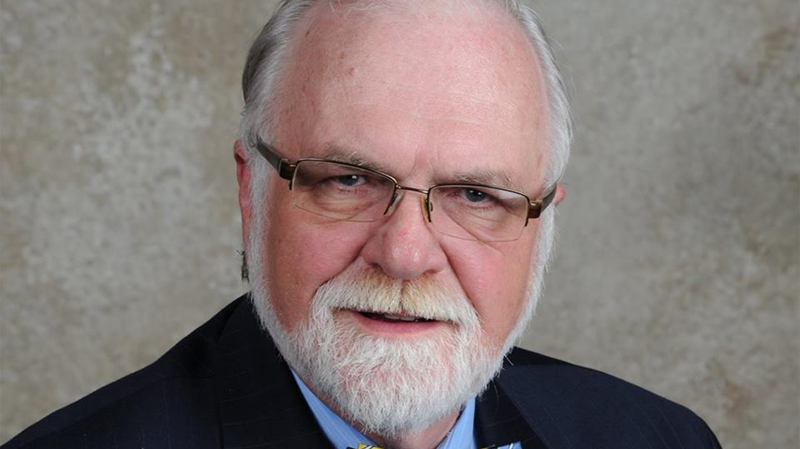
Farrant began advocating for traumatized jurors like himself. And he found an ally in retired justice Patrick Lesage, who presided over the Paul Bernardo trial in 1995.
Lesage had recognized that the graphic nature of the testimony could pose a long-term difficulty for jurors who are not trained to handle extremely violent material. He issued an order to offer mental health help for all jurors in the Bernardo trial.
In 2017, Ontario did finally approve offering mental health services for jurors. Farrant had already found treatment but paid for it out of pocket.
He continues to advocate for jurors at risk of developing PTSD and says while some provinces offer treatment, not all do. He has also been working with the Not Suicide, Not Today campaign by the Centre for Addiction and Mental Health (CAMH).
CAMH researcher and clinician Dr Juveria Zaheer says that while the conversation about mental health has been opening up over the past decade, suicide is still largely unaddressed. And she fears the pandemic may be a new risk factor.
She says, “Some of the risk factors associated with suicide -- social isolation, financial stress, difficulty accessing services, trauma, is what we're seeing in the pandemic.”
Every day in Canada, an average of 10 people die by suicide. And while international suicide figures were reported to be slightly lower at the beginning of the pandemic, she says those figures often lag.
She also says calls to distress lines have risen significantly.
“I think what is happening now is that we know suicide is a preventable outcome,'' says Zaheer.
For Farrant, he says not being able to talk about his mental health struggles compounded his problems.
That’s why he says the Bell Let’s Talk message is so important.
Dr. Zaheer’s message? “We’re going to take this really dark topic and make it public,” she says. “We’re going to say, ‘What is the best we can do to solve this problem together.’”
If you are in crisis, here are some service you can reach out to for help.
Kids Help Phone: Call 1-800-668-6868 or text CONNECT 686868
Wellness Together Canada: visit ca.portal.gs or text WELLNESS to 741741
Black Youth Helpline: Toll Free 1-833-294-8650 (9am to 10pm ET)
First Nations and Inuit Hope for Wellness Help Line: 1-855-242-3310
Canadian Suicide Prevention Service: 1-833-456-4566, Québec Residents: 1-866-277-3553