TORONTO -- Ontario's healthcare system is now at a point at which it may not be able to handle much more than 200 or 300 additional COVID patients in intensive care without considering "other means" to create capacity such as not offering the oldest and sickest patients all care available, a top official at Ontario Health is warning.
The province has experienced exponential growth in both cases and ICU admissions in recent weeks as the deadlier and more infectious B.1.1.7. variant that was first detected in the United Kingdom became the dominant strain.
Last week hospitals outside of northern Ontario were instructed to begin “ramping down” elective surgeries and procedures as of today. Greater Toronto Area hospitals have also been transferring patients to as far away as a Kingston in a bid to free up capacity.
Those measures, however, are only expected to do so much.
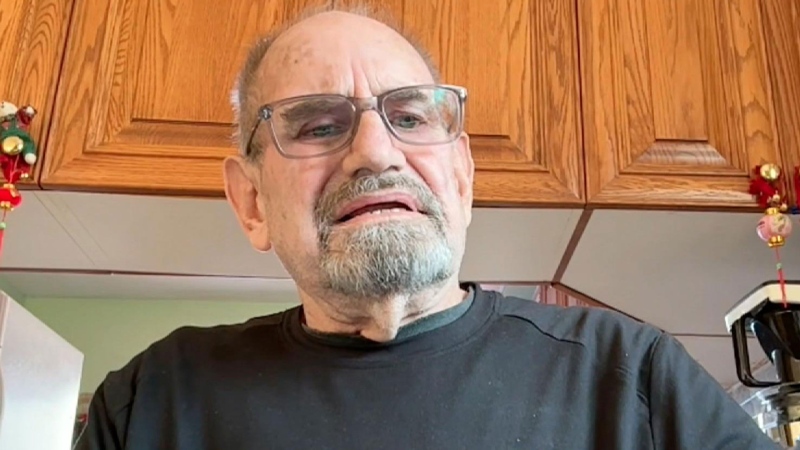
“We are tracking from the 600 COVID patients in ICU today to something like 900 or north of 900 by the end of the month. We think we will be able to do that with these measures. But if we go above that and then COVID numbers in the community continue to grow then we will probably be into territory where we have to start thinking about other means, either growing capacity or activating the triage protocol but that has to be and we are determined that it will be the last resort,” Ontario Health Executive Vice President Dr. Chris Simpson told CP24 during an interview on Monday morning.
There was a total of 619 patients with COVID-19 in Ontario’s intensive care units as of Monday morning, up from 494 at this point last week.
Simpson told CP24 that Ontario Health is “pulling out absolutely all the stops” to avoid having to activate a triage protocol that could see some patients denied care.
He said that “lots and lots of things have been discussed and are on the table” in terms of creating additional ICU beds and, more importantly, finding doctors and nurses to staff them.
But he conceded that “there is a limit” to the measures that can conceivably be done to increase capacity.
Last week, the province ordered doctors and nurses working for Local Health Integration Networks (LHINs) to report to hospitals to offer their services. They also passed a emergency order allowing hospitals to transfer patients without their consent in some cases in order to free up hospital capacity.
“There is only so many healthcare professionals in the province that can be moved around and redeployed,” he warned.
While the province has not yet enacted the triage protocol or announced plans to do so, the College of Physicians and Surgeons of Ontario did send a memo to its members last week to let advising them that they will not be beholden to pre-existing college policies should such a protocol be implemented.
The triage protocol developed by the province in January says that in a scenario where health resources will be exhausted due to the number of patients, those expected to live 12 months or longer post treatment should be given the greatest amount of care and attention.