Millions in taxpayer dollars earmarked for Ontario LTC company that allegedly left residents malnourished
The Doug Ford government says it has allocated hundreds of beds to the Ontario for-profit long-term care chains at the centre of a military report that shocked the nation more than a year ago with details of horrifying conditions and neglect.
Sienna Senior Living, which owns Woodbridge Vista Care Community and Altamont Care Community, two long-term care homes where 84 people died altogether, is in the running to get public funds to build 223 new and 577 redeveloped beds — a move that critics say “rewards” the companies behind the deadliest homes.
In a five-part series, CTV News Toronto is examining the province's decision to allocate new beds and funding to the five companies, guaranteeing their future. Click the link to read the previous installment on Southbridge Care Homes.
PART 2: SIENNA SENIOR LIVING
Nick Puopolo’s heart sank when he saw 10 ambulances parked outside Woodbridge Vista Care Community on one May night during the first COVID-19 wave in Ontario. He said he tried to look inside, past the glaring lights, to see if his mother was inside one of them. The long-term care home, he said, had left him in the dark for weeks and he did not know if she was even alive.
The only information he said he got from the home came from personal support workers (PSWs), who would hurriedly call him and leave quick notes before hanging up, saying the situation was dire, that they needed help and that a single worker would care for 30 residents at a time. He said the staff spoke in secrecy, afraid Sienna Senior Living, the company behind the home, would punish them.
“Nobody was answering our emails and phone calls for two months,” Puopolo told CTV News Toronto. “The only information we were getting was from some of the personal support workers who would call in tears and just tell us what’s happening at the home, saying they were instructed not to tell the family members anything or they would be fired.”
“We planned that if nothing changed and help wasn’t brought in by the end of the week, a whole bunch of us were just going to go there and break the door down.”
The Ontario government did eventually step in during early June, appointing William Osler Health System as the manager of Woodbridge Vista, temporarily removing control of the facility from Sienna. The Canadian Armed Forces were also called to help. The military was already deployed in five other homes at the time, including Sienna’s Altamont home.
Reports offering a glimpse at what military and government inspectors found at Woodbridge Vista only became available at the start of 2021. The home was described as unclean and in a state of disrepair due to damaged walls and flooring as well as a maintenance backlog.
Inspectors confirmed incidences of neglect at the home, including delays in getting residents to hospital when sick and gaps in care related to the collection of testing swabs leading to issues in identifying infection. Inspectors also noted an incident where a resident with COVID-19 was not drinking or eating well, and yet was given a diuretic pill, which can cause people to pass more urine prompting further dehydration. The resident died days later.
 Woodbridge Vista Care Community can be seen in this updated file photo. The home had one of the deadliest COVID-19 outbreaks in Ontario during the first wave of the pandemic.
Woodbridge Vista Care Community can be seen in this updated file photo. The home had one of the deadliest COVID-19 outbreaks in Ontario during the first wave of the pandemic.
Provincial inspectors reported severe staff shortages and that the home had no staffing plan. Workers said they would contact the nurse manager for extra help, but were told, “do the best you can.” Staff described nights where there was only one PSW working. Amid the chaos, inspectors say the home also hired a nurse not qualified to practice according to the College of Nurses of Ontario. The nurse was connected to a neglect case at the home.
The military and province documented issues with supplies at the home, saying that, at times, staff did not have access to equipment for treatments, personal protective equipment or hand sanitizer. Some staff reported they were leaving the home because they had no access to PPE or training.
Puopolo said that even before the pandemic, Woodbridge Vista did not have enough staff to care for residents. He said he hired a private personal support worker to help his mother, who has dementia, three days a week. Once the pandemic hit, he said he panicked because neither he nor the private worker were allowed to enter the home due to the outbreak.
The inspection reports noted that the home failed to communicate with the families of residents and therefore they were unable to participate in the care of their loved ones, leaving them with “disappointment, helplessness, anger and frustration.”
Inspectors said that a doctor told them that, one night in May, several residents were transferred to acute care hospitals all at once because he said, “we were over our heads.” The home was not able to care for residents or monitor them as needed. Woodbridge Vista was not even able to offer or serve residents hot or warm drinks, inspectors noted.
William Osler Health System told inspectors that they offered support to the home on May 4 after hearing from one of its own hospital staff members about the situation. The hospital said that Woodbridge Vista “did not reach out to their community partners for support.” The hospital temporarily took over management of the home on June 4.
In the end, 31 people died at Woodbridge Vista due to COVID-19 alone.
More recent government inspection reports show that some of the issues persist at the Sienna home, including incidents of neglect, inconsistent COVID-19 screening practices, failure to provide residents with safe food and fluid and failure to carry out infection prevention and control programs.
Several of these issues happened as early as June 2021, including incidents where the home got extremely hot in the summer, but residents could not access a designated cooling area. Inspectors found the home had not implemented a heat-related illness prevention and management plan.
“It frustrates me because nothing has changed even after all this time. There's still a staffing shortage, there’s still so many issues,” Puopolo said, adding that he’s currently in the process of getting another private personal support worker for his mother, who still lives at Woodbridge Vista, as she waits for a spot elsewhere.
Puopolo said his mother had to be hospitalized due to COVID-19 and her health has declined significantly since the pandemic.
“She’s not the same person,” he said. “She’s in worse physical shape, because she wasn’t getting proper care for three months so she deteriorated quite quickly. She’s not the same person I saw in January 2020. These people are older, they are elderly, and so when they suffer they don’t come back.”
“Everyone in that facility is not the same as who they were before COVID.”
 Ontario resident Nick Puopolo says his mother had to be hospitalized due to COVID-19 and her health has declined significantly since the pandemic. (Supplied)
Ontario resident Nick Puopolo says his mother had to be hospitalized due to COVID-19 and her health has declined significantly since the pandemic. (Supplied)
MORE MONEY, BEDS FOR SIENNA DESPITE 471 PEOPLE DEAD
As part of its most recent budget and campaign promise, the Progressive Conservative government has promised to add 30,000 new long-term care beds over the next 10 years, adding that 20,161 new and 15,918 upgraded beds are in the “development pipeline.” After Sienna Senior Living applied for some of those beds, the government allocated the company 223 new and 577 redeveloped beds.
Sienna can use its allocations to build long-term care home projects, which would undergo a consultation process before being finalized. The province has so far granted and finalized 30-year licenses and tens of millions of taxpayer's dollars for two 160-bed Sienna homes in North Bay and Brantford, Ont.
The Ontario Ministry of Long-Term Care told CTV News Toronto that the pandemic has displayed the urgent need to update homes to prevent the spread of outbreaks and will add capacity to areas of the province with “significant demand.”
“The ministry’s evaluation process prioritized redevelopment of older homes to implement the lessons learned on improved infection prevention and control measures, particularly the elimination of three and four bed ward rooms, in which isolation and cohorting has proven difficult,” a spokesperson said.
“New spaces built to modern design standards will help prevent and contain the transmission of infectious diseases and ensure residents have access to the care they need in a safe and secure environment.”
The province’s latest round of applications for long-term care bed allocations closes on Nov. 2, 2021. The applications are open to all for-profit, not-for-profit and municipal operators.
In a news conference on Tuesday regarding the Ontario government's plans to spend $20 million to double the number of long-term care home inspectors in the province, Long-Term Care Minister Rod Phillips did not provide an answer when asked why the long-term care homes listed in the military report have not received penalties.
Advocates, families and experts are calling on the government to stop giving more public funds to for-profit companies with a history of violating the Long-Term Care Homes Act, and instead offer those "rewards" to the homes and companies that were praised for their response to the COVID-19 pandemic, and had no deaths.
According to government data, across the province, at least 471 people died in the 37 homes owned by Sienna Senior Living during the COVID-19 pandemic.
While residents at Sienna's homes faced horrifying conditions and neglect as noted in military and inspection reports, the company paid $15.69 million to shareholders from April to June during the first wave. The home continues to pay millions to shareholders, while at the same time taking taxpayers dollars to build more beds.
“They abused people and now they are going to get more beds,” Puopolo said. “I don't think the government should be giving any for-profit long-term care corporation a license for any more beds. If the military or a hospital was brought to run or help at one of their facilities, it tells me they don't have the skills to run a facility.”
 Altamont Care Community is seen in this photo. A staff member at the Scarborough long-term care home has died from COVID-19.
Altamont Care Community is seen in this photo. A staff member at the Scarborough long-term care home has died from COVID-19.
A spokesperson for Sienna Senior Living told CTV News Toronto that it is focused on modernizing their older care communities and that the government support is vital for that.
“The ongoing support provided to all long-term care homes by the provincial government is critical to the sector,” a spokesperson said in an emailed statement. “Adding additional beds, where possible, to our new care communities will help improve access for the thousands of seniors who are currently waiting for long-term care.”
The spokesperson continued to say that the long-term care homes assisted by the military were “hit badly at the beginning of the first wave of COVID-19, before masks, social distancing, and many of the impactful measures became standard practice.”
At Altamont Care Community, one of the homes at the centre of the Canadian Armed Forces first report on long-term care, 53 people died due to COVID-19 alone, but it is not yet clear how many people died due to other reasons such as neglect or hunger. CTV News Toronto asked Sienna Senior Living about the issue, but did not receive a response to this inquiry.
The military report about the home, written by Brigadier-General C.J.J. Mialkowski, found that most residents at Altamont were not fed three meals a day due to staffing shortages and that “poor nutritional status was reported” due to the underfeeding.
The military said that when they arrived at Altamont, they found many residents had been bed bound for several weeks and many residents had pressure ulcers due to the prolonged bed rest. They wrote that they saw no evidence that residents were being moved to wheelchairs for parts of the day, repositioned in bed or washed properly.

“Significant number of residents have pressure ulcers, stage two, three and four and unstageable as a result of prolonged bed rest,” Mialkowski wrote. “Wound dressing orders have not been updated nor adhered to by agency staff causing further degradation of wound.”
The Ford government initially refused to call in the armed forces in early April, saying they felt military aid wasn’t yet necessary despite the reports of severe staff shortages. If the government had sent in the military sooner, critics say more lives could have been saved. The details in the military report gave the public a first official glance in May 2020 at what was happening inside Altamont.
In the military report, Mialkowski wrote that scheduling and staffing was a significant concern at the long-term care home. He said he noticed that, many times, no personal support workers were present after 2:30 p.m., and that, often, one of these workers were caring for 30 to 40 patients at a time, allowing them to only complete the most basic daily requirements, but no ability to provide “nail care, skin care, repositioning or adequate wound care.”
In addition, they said that residents who got hungry around 3 a.m. would be told to have a cookie, some cold coffee or wait until morning because the kitchen was closed to workers at night. The military said they would give their own personal food to ensure residents didn’t go hungry. A resident inside the home during the pandemic told CTV News Toronto he could hear wailing inside the rooms at night for long periods as people called for help.
‘THE MOST HORRIFYING THING I HAVE EVER SEEN’
Ontario’s long-term care sector underwent significant change in 1998, when former Conservative Premier Mike Harris announced his government was awarding 20,000 new licences for long-term care beds. While not-for-profit churches and charities had dominated the industry before then, the majority of the new licenses were given to for-profit companies.
Now, 58 per cent of long-term care homes belong to for-profit companies in Ontario, a number unseen anywhere else in Canada.
According to data collected by the Ontario Health Coalition, the COVID-19 death rate during the pandemic involving for-profit long-term care homes in the province is about nine per cent; comparatively, in not-for-profit homes it stood at 5.25 per cent and, in publicly-owned homes, the number dropped to 3.62 per cent.
Scientists advising the government on the COVID-19 pandemic have stated that for-profit homes had nearly twice as many residents infected with the virus and 78 per cent more deaths compared to non-profit homes. Ontario's own long-term care commission, which investigated how and why the coronavirus spread in nursing homes, stated in its final report that the for-profit aspect of the sector needed to be revisited.
Natalie Mehra, the executive director of the Ontario Health Coalition, said that, at the very least, the Ford government should not provide public funds to the companies with the worst records and violations, including those visited by the military.
“Why would we be paying for-profit companies especially those with hideous records to be building the next generation of long-term care homes? It’s absurd,” she said. “More than 4,000 people are dead and that's not in keeping with the rest of the world, like no one else saw death rates like we saw in Canada in long-term care homes.”
In order to build and redevelop beds, long-term care operators are currently paid a development grant and a construction subsidy, which is a per day payment for the 30 years of the license term.
The construction subsidy is based on a project’s location and size. It can range anywhere between $20.51 to $23.78 per day, plus $1.50 per bed for homes with 96 beds or fewer and $0.75 per bed for homes with 96 to 160 beds.
Long-term care corporations also get a capital development grant, which can range anywhere between $29,246 and $51,376 per bed depending also on where it is located and size. Larger homes in urban centres get the most money.
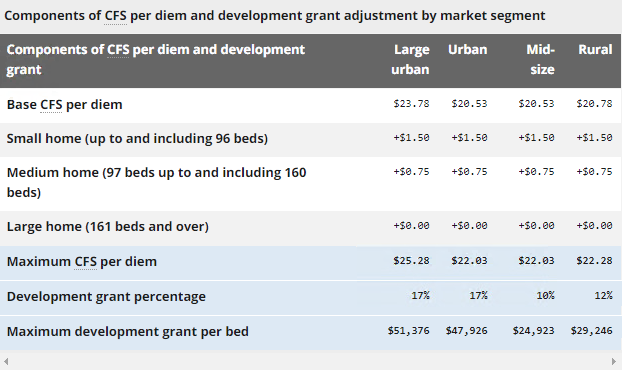 Mehra told CTV News Toronto that a 200-bed home built in a large urban centre could provide a corporation with $10.26 million through the capital development grant and $52.1 million through the construction funding subsidy.
Mehra told CTV News Toronto that a 200-bed home built in a large urban centre could provide a corporation with $10.26 million through the capital development grant and $52.1 million through the construction funding subsidy.
At the same time, a company can also charge residents anywhere between $1,891.31 and $2,701.61 per month for accommodation at a long-term care home.
“I don't know how, in any way shape or form, you can justify, providing more money and more licenses to homes that were occupied by the military, that had some of the most disastrous outcomes,” Dr. Vivian Stamatopoulos, a long-term care advocate, told CTV News Toronto.
“I mean, we have the documents and evidence of which home, which chains of homes were the worst offenders. They got away with murder and they are just helping these very profitable companies become very wealthy.”
“You’re rewarding those very bad actors for with another generation of licenses. It is the most horrifying thing I have ever seen.”
FORGOTTEN: Part three will be released tomorrow on CTVNewsToronto.ca
CTVNews.ca Top Stories

Widow looking for answers after Quebec man dies in Texas Ironman competition
The widow of a Quebec man who died competing in an Ironman competition is looking for answers.
Tom Mulcair: Park littered with trash after 'pilot project' is perfect symbol of Trudeau governance
Former NDP leader Tom Mulcair says that what's happening now in a trash-littered federal park in Quebec is a perfect metaphor for how the Trudeau government runs things.
World seeing near breakdown of international law amid wars in Gaza and Ukraine, Amnesty says
The world is seeing a near breakdown of international law amid flagrant rule-breaking in Gaza and Ukraine, multiplying armed conflicts, the rise of authoritarianism and huge rights violations in Sudan, Ethiopia and Myanmar, Amnesty International warned Wednesday as it published its annual report.
Photographer alleges he was forced to watch Megan Thee Stallion have sex and was unfairly fired
A photographer who worked for Megan Thee Stallion said in a lawsuit filed Tuesday that he was forced to watch her have sex, was unfairly fired soon after and was abused as her employee.
Amid concerns over 'collateral damage' Trudeau, Freeland defend capital gains tax change
Facing pushback from physicians and businesspeople over the coming increase to the capital gains inclusion rate, Prime Minister Justin Trudeau and his deputy Chrystia Freeland are standing by their plan to target Canada's highest earners.
U.S. Senate passes bill forcing TikTok's parent company to sell or face ban, sends to Biden for signature
The Senate passed legislation Tuesday that would force TikTok's China-based parent company to sell the social media platform under the threat of a ban, a contentious move by U.S. lawmakers that's expected to face legal challenges.
Wildfire southwest of Peace River spurs evacuation order
People living near a wildfire burning about 15 kilometres southwest of Peace River are being told to evacuate their homes.
U.S. Senate overwhelmingly passes aid for Ukraine, Israel and Taiwan with big bipartisan vote
The U.S. Senate has passed US$95 billion in war aid to Ukraine, Israel and Taiwan, sending the legislation to President Joe Biden after months of delays and contentious debate over how involved the United States should be in foreign wars.
'My stomach dropped': Winnipeg man speaks out after being criminally harassed following single online date
A Winnipeg man said a single date gone wrong led to years of criminal harassment, false arrests, stress and depression.