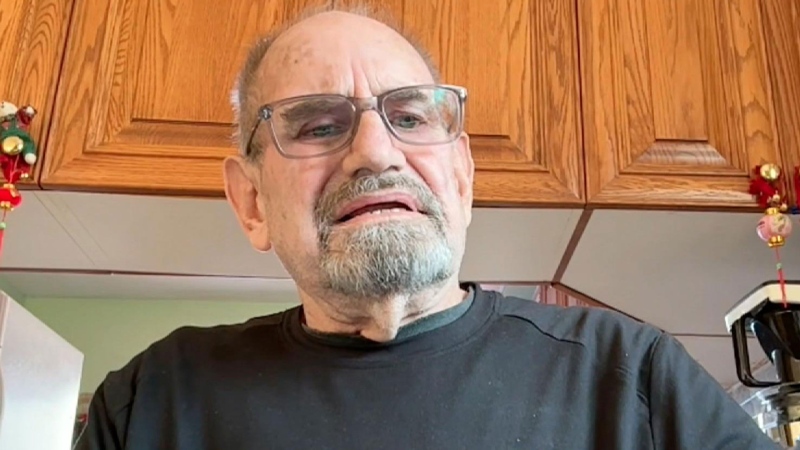
An Ontario man who winters in Arizona was shocked recently after receiving a $26,000 bill for a three-day hospital stay in the U.S. despite having travel insurance.
Edward Ing told his insurance company prior to heading south that he had a heart condition and high blood pressure. In February, while in Arizona, Ing felt lightheaded and dizzy and went to a local hospital.
Ing says he told hospital administrators that he didn't want any treatment until they checked his insurance plan to ensure he would not get stuck paying the bill.
According to Ing, the insurance company gave the hospital the go-ahead to run multiple tests. Ing was also held for three days at the hospital before being released with a clean bill of health.
Approximately a month later, Ing received an expensive bill for the tests and hospital stay.
"That's when I phoned them and said, 'This is going to give me a heart attack for the tests because I thought it was covered,'" he told CTV Toronto.
Ing has since appealed to the Royal and Sun Alliance Insurance's ombudsman about his bill.
According to the company's coverage policy, however, a claim can be denied if an individual has consulted with a specialist -- something Ing did last year when his doctor suggested a procedure that would help stabilize his heartbeat.
The company's policy states: "There has been no hospitalization or referral to a specialist (made or recommended) and there is no further investigation for which results are pending."
A spokesperson for Royal and Sun Alliance Insurance said they are investigating Ing's appeal.
"We ensure that in any appeal we follow rigorous due diligence processes in the validation of the policies, terms, conditions and exclusions," the spokesperson said.
Ing expects to find out if his appeal will be denied in the coming days.
With a report from CTV Toronto's Pat Foran