TORONTO - A decades-old antibiotic appears to work better when combined with a common antidiarrheal drug to combat a persistent bug that often afflicts people with cystic fibrosis, a new study indicates.
The synergy between the two drugs was discovered in lab studies by researchers at McMaster University in Hamilton who have been screening chemicals in search of combinations of molecules that might have an impact on the growth of bacteria.
Bacteria have become resistant to a lot of antibiotics used to fight infection in cystic fibrosis patients, said Maureen Adamson, CEO of Cystic Fibrosis Canada, a charity that helped fund the research.
"So we're constantly looking for new ones and as you know, it takes a very, very long time to bring a new drug to market. So this research is looking at existing drugs and ... it could cut (the) time in half," she said.
"For people with cystic fibrosis, frankly, time is of the essence."
In this case, the research team got its results in lab dishes and a mouse study by combining the antibiotic minocycline and loperamide, more commonly known as Imodium.
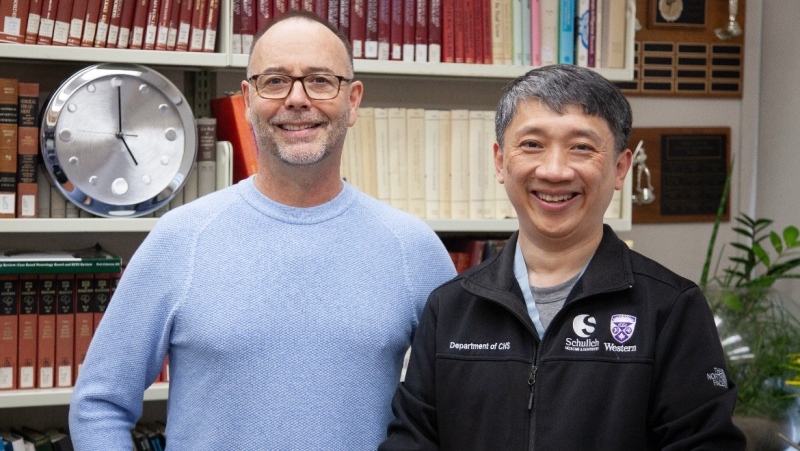
"We showed basically in a Petri dish or in a test tube, if you will, that loperamide in combination with minocycline had antibacterial activity," said Prof. Eric Brown, who worked on the project with Gerard Wright, Brian Coombes and other colleagues in the department of biochemistry and biomedical sciences.
"Imodium, of course, is a molecule that actually has an impact on gut motility, and is not been known before to have any antibacterial activity."
On its own, he described minocycline as a relatively mediocre antibiotic.
Due to resistance issues, it's not used to fight Pseudomonas aeruginosa -- a bacterium that's a problem for CF patients who get lung infections, said Bob Hancock, a University of British Columbia professor who wasn't connected with the study.
This particular drug combo has potential, he said, but more importantly, the approach that involves screening more than 1,000 different drugs in combination has "massive potential."
"I think the approach is really exciting and it has a potential to breathe new life into antibiotic discovery, and we desperately need that," said Hancock, a researcher at the Centre for Microbial Diseases and Immunity.
Multidrug-resistant Pseudomonas is now officially a superbug, so a variety of treatments are needed, he indicated.
"Companies are falling out of antibiotic research like fleas off a dog. So in the '80s we had 36 companies doing antibiotic research. I think we're down to about six," Hancock said.
"It's a tragedy. We have 100,000 people dying in North America from antibiotic-resistant infections every year, and a third of the world's population die of infections, so we can't really afford to lose more when the resistance is rising."
The McMaster study was published Sunday in the journal Nature Chemical Biology.
Brown said complicated bacterial physiology is involved in this combination, but the loperamide appears to disturb membrane potential, and in the process, the minocycline molecule gets into the cell better.
Although it was only shown in a Petri dish, he said that with antibiotics, whatever works in a dish is often predictive of what would happen in a human infection system. In the animal model, minocycline alone had a modest effect against salmonella, and Imodium alone did virtually nothing. But together the two molecules showed "remarkable synergy" in clearing salmonella infection, Brown said.
Because loperamide and minocycline have been around for years and studies on the drugs already exist, it would shorten the timelines for any potential combo drug.
"It's estimated that it takes 13 to 15 years and a billion dollars to discover a drug, and if you think about the steps that we're trying to leapfrog, then maybe that time could be cut in half or so," Brown said.
He indicated some other promising drug combinations -- anti-fungal and anti-MRSA -- have shown up in his research as well, and he thinks they're just "the tip of the iceberg." MRSA is methicillin-resistant staphylococcus aureus, a bacterial infection that often sickens hospital patients and is highly resistant to many antibiotics.
Hancock said when a combination of already-approved drugs is used, clinical trials are still needed because you have to be sure the drugs don't interact with each other in a negative fashion.
"They have to be applied in a certain way at a certain dosing to ensure that the concentrations of the drug are adequate for therapy over the course of treatment," he said.
"It would take a while to figure out how to combine them, so it might be that one drug is taken best before meals and another drug after meals. You can see that there's a lot of different things that have to go into figuring out exactly how to apply combinations, as opposed to an individual drug."
Brown received $163,500 in funding from Cystic Fibrosis Canada to support the research and $89,775 is committed for further investigation. In addition, his collaborator Wright is receiving $125,000 from the charity for his research on antibiotic adjuvants.